The Focus Paper “Primary care: a challenge for the National Health Service” analyses the component of the NRRP devoted to primary care, for which EUR 7 billion in investments and EUR 500 million from the Complementary Fund (Fondo complementare, FoC) are earmarked. The Plan calls for an important effort to reorganise non-hospital healthcare, a crucial step in upgrading the Italian National Health Service (NHS), and to reorganise the prevention system.
In recent years, one of the most widespread policies adopted in European countries to improve healthcare services has been to shift the focus away from hospitals towards primary care. In Italy, however, the downsizing of hospital capacity – which was already low compared to other countries (the number of hospital beds per 1,000 inhabitants fell from 4 in 2005 to 3.2 in 2019, while the European average fell from 6.1 to 5.3) – was not accompanied by an adequate strengthening of primary care, whose shortcomings are more evident in certain regions.
Despite the fact that the new system of primary care had long been envisaged in its basic outlines, and that a number of relevant experiences had been carried out in a number of regions, proximity health facilities or the associations of general practitioners – offering services in wide time slots – have rarely become effective points of reference for citizens, and many regions, especially in the South of Italy, do not have intermediate facilities for inpatients requiring low-intensity clinical interventions. This means, among other things, that hospitals are often overwhelmed by requests for procedures that could be performed elsewhere.
Funding under the NRRP
To address this situation, the primary care interventions to be financed by the NRRP are structured on three levels: Community Health Houses (i.e. proximity facilities, aimed at referring patients to primary health care and social care services, dealing with health promotion, and ensuring the care of chronic patients), for which EUR 2 billion have been allocated; Community Hospitals, for which EUR 1 billion has been earmarked; Home Care, with resources amounting to EUR 1 billion for telemedicine, EUR 2.72 billion to increase the number of over-65 patients by at least 800,000 and bring it to 1.5 million, and another EUR 280 million to activate 600 Territorial Coordination Centres (Centrali Operative Territoriali, COT) by June next year. All these services will be included in the new organisational model for the primary care network outlined in the dedicated reform, aimed at determining structural, technological, and organisational standards, as well as introducing a new institutional structure for health, environmental, and climate prevention (whose funding is directly financed by the Complementary Fund).
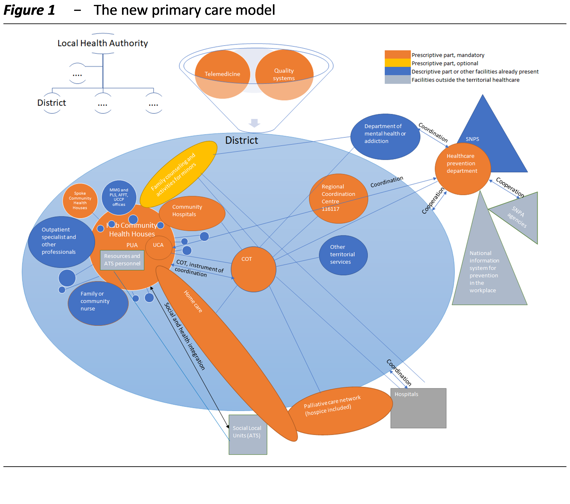
Figure 1 provides an overall and stylised view of the network of services and structures that will make up this new model, as well as of the main interrelationships between the different components, the essential features of which have been defined in the Regulation introduced by Ministerial Decree 77/2022, which carried out the reform envisaged by the NRRP. The figure shows the key elements of the new primary care assistance network (in orange the mandatory structures regulated by the prescriptive part of the law, in yellow the optional ones, in blue those referred to in the descriptive part or in any case already present, in grey those outside the primary care system).
The distribution of funds
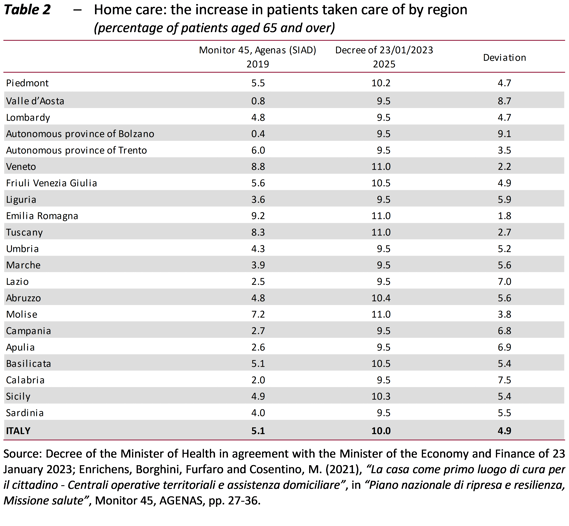
Of the earmarked EUR 7 billion, EUR 6.675 billion were to be distributed among the regions and autonomous provinces. The funds distributed to date amount to EUR 5.9 billion, of which 42.8 percent went to the South of Italy (Table 1). Efforts were made to render the constraint allocating 40 percent of the resources for southern regions more flexible, by applying specific criteria for the various investments (the parameter of one COT per 100,000 inhabitants, the increase to 45 percent of the quota for southern regions to take into account the different needs for Community Health Houses, the incidence of the elderly together with the target of 10 percent of over-65 population for home care in all regions).
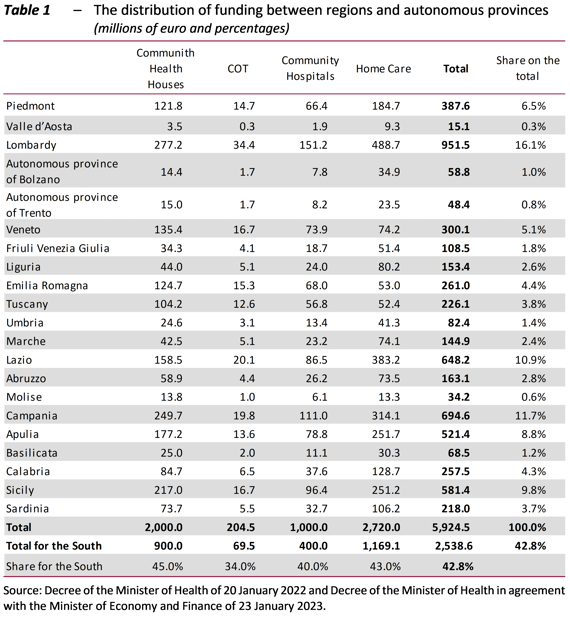
However, significant territorial imbalances may remain in the availability of Community Health Houses and Community Hospitals and, with regard to home care, the more advanced regions have demanded compensation in the face of an allocation of resources aimed at achieving uniformity (Table 2). To even out the quantity and quality of services in the country, a collective effort must be made to guarantee more resources to the weakest areas.
The FoC-funded investment addresses the reorganisation of the health, environmental and climate prevention system: in this case, EUR 399 million out of EUR 500 million will go to local authorities.
The critical aspects of the reform
An analysis of the reform of the primary care and the prevention systems, contained in Ministerial Decree 77/2022, reveals three main critical issues:
-
- Some doubts remain as to the assessment of the current resources needed to make the new primary care structures operational. Moreover, once the NRRP resources are exhausted, more than EUR 1 billion will have to be recovered in NHS funding to provide continuity for home care services and, once the Community Hospitals are operational, EUR 239 million will have to be found to pay their personnel. In addition, the financial planning for the three-year period beginning in 2023 implies a downsizing of the share of the GDP allocated to public health, which would make it difficult to strengthen services, even if they are reorganised. Therefore, it is plausible that there will be a need to allocate additional funding for primary care; furthermore, the Government has committed to the regions to find additional resources should they become necessary, compatibly with public budget constraints. With regard to the necessary increase in human resources, the difficulty in finding personnel and the loss of attractiveness of the NHS are becoming a pressing issue, especially with regard to nurses and certain categories of physicians. This must be addressed through adequate personnel planning, an increase in the training offer, and the adoption of measures aimed at restoring the appeal of working in the NHS in terms of social and economic status.
-
- The involvement of general practitioners (GPs) in the implementation of the reform would require a clear regulation of the forms and methods of their participation in the various structures and a revision of the training programmes in order to strengthen them and adapt them to the new primary care system in the territory. The hypothesis of transforming general practitioners from contracted freelancers into NHS employees seems to have been shelved for the time being. The 2019-21 Guideline Act for the national agreement with GPs emphasises the role of GP aggregations more than that of Community Health Houses and merely assumes that the reorganisation that has emerged from previous agreements is already consistent with the provisions of the NRRP and adaptable to the new Regulation containing the standards of primary care (Ministerial Decree 77/2022). The delay in national bargaining on wage increases – the agreement under discussion today refers to a period that has already expired – ends up being the cause and effect of the difficulties in introducing and financing more relevant innovations, which are also necessary in the light of the reform.
-
- The new Regulation of primary care is the instrument for ensuring uniform standards throughout the country, but the institutional innovations will have to be dropped into the individual regional models. Ministerial Decree 77/2022, in the final version of which the prescriptive part has been better identified, but also delimited, leaves many solutions open, also with regard to the role of the private market, which may find rather wide room for expansion depending on the implementation choices of the Regions. In order to prioritise the planning function, maintaining on the one hand control over expenditure and on the other hand a commitment to appropriateness and fairness in the provision of services, the role that the District will assume, emphasised in the descriptive part of the Regulation and strengthened by recent measures, appears all the more important.
Lastly, it should be noted that a number of important aspects of the reform are still being defined: the integration with the social services managed by the social local units (ambiti territoriali sociali, ATS), whose staff will have to be present in the Community Health Houses, and between the National System for the prevention of health against environmental and climatic risks (Sistema nazionale prevenzione salute dai rischi ambientali e climatici, SNPS), established by Legislative Decree 36/2022, and the System for environmental protection (Sistema di protezione dell’ambiente, SNPA). The latter is also relevant in view of the recent constitutional reform, which introduces environmental protection and sets limits on private economic activity in relation to the environment and health.
Text of document (in Italian)
